
There is hardly a person who at least once in his life will not experience back pain in the lumbar region. This is how we pay for walking upright and our daily habits.
In addition to damage that can affect the spine, muscles, nerves and ligaments, it should be remembered that sometimes the back hurts in the lumbar region with internal diseases - diseases of the kidneys, gastrointestinal tract, and female genital organs.
Low back pain symptoms can range from dull to sharp. The pain may go away on its own or become chronic (symptoms have been present for more than three months).

danger! You should see a doctor immediately if:
- pain in the lumbar region arises suddenly after an obvious back injury;
- the temperature has risen sharply, there are vegetative disorders, loss of consciousness, sweating, difficulty breathing;
- Involuntary bowel and bladder emptying occurs;
- there is numbness in the groin area;
- there is weakness in the lower part of the legs, their paresis or paralysis, impaired sensitivity;
- pain is given to the stomach and increases sharply when coughing or sneezing;
- symptoms appear against the background of sharp weight loss, prolonged use of steroids, immunodeficiency;
- in the family history there are cases of cancer, inflammatory or degenerative diseases of bones and cartilage tissue.
Why back pain in the lumbar region?
Myofascial pain
Muscle tension or spasms can develop gradually or occur suddenly. With high loads, the damage affects not only muscle fibers, but also ligaments and fascia.
Muscle pain in the lower back appears after:
- lifting heavy weights or overexerting yourself at work or playing sports;
- exercise from time to time. Muscles are especially vulnerable if you are inactive during the work week and then spend hours in the gym at the weekend;
- a sudden increase in own body weight, behind which the muscles do not have time to develop;
- sitting or standing for long periods in an uncomfortable position;
- every day carrying a bag in one hand or over the shoulder;
- posture disorder. The spine performs its best support and protection functions when you are not bending over. The muscles in the lower back experience the least stress when you sit with good support under your lower back, and in a standing position, distribute the weight evenly on both legs.
If the back hurts after bruises, fractures, sprains, hypothermia, infectious diseases or established helminthic invasion, then myositis (inflammation) of the muscles of the lower back can be suspected. Severe pain is always present due to inflammation of muscle fibers, "nodules" are felt in the muscles - places of spasms. Inflammation can be acute or take a chronic form. With a long course of the disease, the pain is unstable, aggravated by lying down or sitting for a long time, in the late evening or when the weather changes. Touching the muscles causes pain and discomfort, the muscles of the lower back are in constant tension, inflammatory edema is formed, the temperature rises locally and at the level of the whole organism.
With muscle spasms, the roots of the spinal nerves are violated, so the attack often resembles a picture of sciatica or sciatica - there is a severe burning pain along the back of the thigh and lower leg, the limbs become numb, they lose sensitivity. The clear muscle tone in myositis makes the patient take a forced position, he walks and lies bent over, moves on bent legs.
How to treat spinal muscle pain? Nonsteroidal anti-inflammatory drugs and analgesics are used to eliminate inflammation and pain. Medicines can be taken in the form of tablets, ointments, injections, transdermal patches with gradual release of active ingredients. Irritating and warming ointments are also used, which reflexively increase blood flow to the muscles of the lower back. The larger amount of blood that flows contributes to the cleaning of inflammatory products and tissue damage.
Reduction of inflammatory edema is facilitated by corticosteroid injections and vasoconstrictive drugs.
If the cause of myositis is infection or body poisoning with worm toxins, then initially antibiotics or anthelmintic drugs are used. In this case, warming ointments or compresses should not be used.
Diseases of the spine that involve nerve endings
In the lumbar region, the vertebrae are separated by elastic cartilaginous discs, which protect the spine from injury, but they themselves are subject to wear and aging.
Normally, the disc is a jelly-like nucleus pulposus surrounded by a denser layer of annulus fibrosus. The elasticity of the core is due to its ability to bind and retain water: when the load increases, it accumulates water, and elasticity increases, when the pressure decreases, the core releases water and becomes flatter.
Osteochondrosis in the vertebral region develops when the intervertebral disc is undernourished ("drying") or with excessive local load. Often, lower back pain is caused by the fact that the lower pole of the intervertebral disc bears the greatest load when sitting, when lifting weights in front of it. At the same time, tears, displacements are formed in the disc, vertebral ligaments are damaged, there is constant pain, throbbing.
Pain in the spine has several mechanisms of development:
- violation of microcirculation in the tissues around the spine and, in particular, in the spinal canal, the formation of congestion and edema. Such conditions develop against the background of hypothermia, overheating, inflammatory processes.
- degenerative process in the ligaments fixing the spine. An increase in the mobility of the vertebrae leads to a slight displacement and non-physiological compression, which causes the violation of nerves, blood vessels, and the formation of hernias.
- compression of the vertebral axis when lifting weights or damaging it during excessive rotation (twisting).
- aseptic inflammation. Destruction of the nucleus leads to the release of sensitizing factors into the spinal canal. There is irritation at the nerve endings, which causes muscle spasms that violate neighboring vertebrae - above and below the hernia. Gradually, the reaction covers the entire lumbar region and leads to the fact that any movement causes a sensation of pain.
A weakened disc can rupture, resulting in bulging, protrusion, or prolapse of the nucleus, and eventually herniation. The appearance of a hernia puts pressure on the spinal cord and spinal cord roots. In such a situation, throbbing pain in the lower back appears suddenly, which deviates along the strangled nerve. The most famous cases of compression of the sciatic nerve (sciatica), manifested by sharp pain along the back of the thigh and lower leg, numbness of the limb from the side of the hernia, muscle weakness, involuntary pinching. legs.
Pain in the lumbar spine worsens in a sitting and standing position, when turning, leaning. Often there is a protective muscle reaction - painful muscle contraction (roller formation) on both sides of the spine, which isolates the department from unnecessary movement. Osteochondrosis further leads to the appearance of sciatica (inflammation of the spinal nerve root).
Radicular syndrome is dangerous when the nerves of the lower back, which are responsible for innervation of internal organs (cauda equina horn), are pinched. At the same time, pain is given to the stomach, bladder and bowel functions are disturbed, there are problems with potency in men and gynecological diseases in women.
Many patients, due to the fact that the lower back is very painful, take an analgesic posture - they deviate to the left, if the right side hurts, lie on the right side. If the hernia is on the left side. Also characteristic is the appearance of severe pain when pressing the hernia in the intervertebral space (ringing symptom).
How to treat if your back hurts with osteochondrosis:
- during an attack of pain, you can take an anesthetic pose - lie on your back, and put a roller under your knees. It is also recommended to sleep on a hard surface;
- of analgesic drugs, NSAIDs can be taken orally or as an injection on both sides of the spine at the lumbar hotel;
- use local irritants as a nuisance therapy - mustard plasters, iodine mesh, pepper patches and ointments;
- eliminate miotic spasms through manual therapy, acupuncture, vacuum massage, reflexology, gymnastics;
- during the reduction of the acute period, mud treatment, ozocerite, heating can be used.
Pain treatments in radicular syndrome include:
- providing bed rest, lumbar traction (dry or under water);
- the use of novocaine blockade at the site of violation, the use of NSAIDs or weak opiates;
- physiotherapy - microcurrent stimulation, electrophoresis with analgesics.
Indications for surgery are persistent acute pain, as well as dysfunction of internal organs, the development of paralysis of limbs, absorption of hernias in the spinal canal.
Degenerative inflammatory lesions
Spondylarthrosis (inflammation of the vertebral facet joints) occurs with degeneration, a decrease in the height and volume of the intervertebral disc. Pain in the lower back appears due to excessive stretching of the capsule and increased pressure on the intervertebral joint surface. The pain causes the patient to bend more in the lower back, thereby increasing the load on the intervertebral joints. Especially the discomfort in the lower back is aggravated by wearing shoes with heels, walking for a long time, getting off an elephant, positions when the body is turned backwards, for example, when looking at something overhead.
In patients with this diagnosis, stiffness in the lower back is noted in the morning, the pain increases during the day or after exercise. It has a diffuse character and it is difficult to show the boundaries clearly: discomfort is determined in the gluteal muscles, inguinal area, lower abdomen, and in the scrotum in men. This spondyloarthrosis differs from radicular syndrome, when you can determine the cause of the pain.
What should be done to relieve the pain? It usually helps to take a supine position, bending the legs at the hip and knee joints.
Their medication is a choice of non-steroidal anti-inflammatory drugs and non-narcotic analgesics.
Muscle relaxation is also added as it relieves muscle tension and improves spinal mobility.
Psychotherapy has a positive effect, because chronic pain introduces the patient into a state of depression.
Spondylosis, unlike osteochondrosis, affects the fibrous ring of the intervertebral disc and the anterior longitudinal ligament more. With this disease, calcification of connective tissue structures occurs with the formation of growths along the edges of the vertebrae - osteophytes. This formation causes a violation of microcirculation near the nerve roots and leads to the fact that the back hurts in the lower back, and the mobility of this department is also limited.
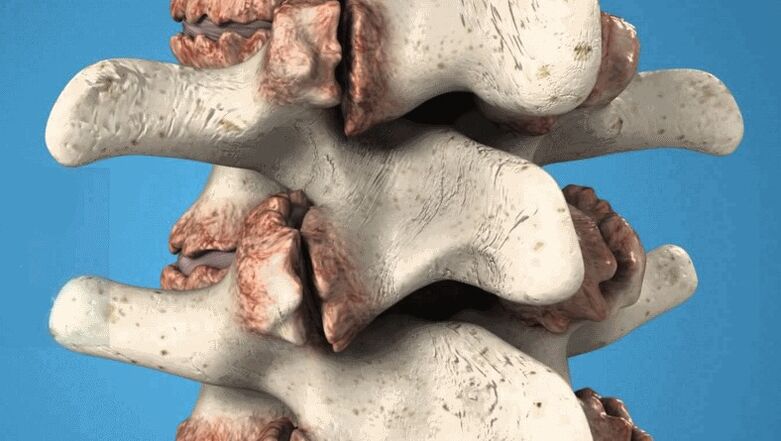
Vertebral osteophytes are pathological growths that damage nerves and blood vessels.
Treatment is usually conservative, with the use of anti-inflammatory drugs, analgesics, vitamins. A good effect is given by electrophoresis with novocaine, lidase, manual therapy, physiotherapy (amplipulse, laser installation, shock wave therapy to destroy dense elements and increase spinal mobility).
Notes! In advanced stages, osteophytes cannot be resolved. Despite its small size, the treatment aims to eliminate inflammation, pain, and improve metabolism. If the back does not hurt too much, then nothing is done with the tumor. If the osteophyte causes persistent or significant pain, it can be removed during surgery.
Diseases that are tumors
Back pain can occur as a result of compression of the spinal cord by tumors from the outside (extramedullary formation) and from the inside (intramedullary, originating from the cerebrospinal substance itself).
Cells of various tissues can grow pathologically:
- fatty - lipoma is formed;
- nerve root - neuroma;
- spinal cord - hemangioma;
- additional tissue - glioma;
- bone tissue - osteosarcoma;
- cartilage - chondrosarcoma.
The tumor process, especially malignant, is characterized by a pain syndrome resembling sciatica (it can be unilateral and bilateral), a general deterioration in the patient's condition, and fatigue.

If the pathology affects the I-IV lumbar vertebrae, then there is a burning pain in the front and on the side of the upper thigh, incomplete paralysis in this area.
With lesions in the lumbar area IV - II sacral segment, numbness of the paragenital area, motor disorders and sensory conservation of gluteal muscles, posterior thigh, calf, stool and urinary incontinence are observed.
Obvious disturbances in the function of the pelvic organs occur with neoplasms in the area of the V-III sacral vertebrae. Patients experience sexual impotence or menstrual disorders, constipation or faecal and urinary incontinence.
Tumor treatment is specific, painkillers, and anticancer drugs are prescription drugs.
As you can see, lower back pain is usually caused by musculoskeletal pathology. They can be diagnosed with clinical signs and research data, the main task is to correctly determine the nature of the disease and not to confuse it with oncological causes, diseases of internal organs or trauma. If you suffer from back pain, we recommend that you always seek the advice of a neurologist or orthopedist.

















































